Starting IVF can feel overwhelming. When we began our own journeys, there were so many things we wish we had known beforehand—things that would have helped us feel more in control and prepared. Every clinic is the same, right? We’ll probably get pregnant after the first or second try!
That’s what we naively thought when we started.
Little did we know it would take more than 17 IVF cycles between us and 30 embryos to finally get our miracle babies — or that we’d end up spending every waking hour researching anything that might give our next cycle a better chance.
That’s why we created this platform—to share insights, tips, and lessons we learned along the way so you can feel more prepared than we were when starting your IVF journey.

1. IVF Doesn’t Always Go as Planned
While IVF has helped millions of people become parents, it’s not a guaranteed success. We thought we’d get pregnant after one or two tries but soon found out this would not be our story.
You might not get pregnant right away. Or you might get pregnant, but not stay pregnant. Both are deeply painful. IVF is full of unknowns—and emotionally, that’s one of the hardest parts.
Even when you finally get that second pink line, the anxiety doesn’t disappear. You’ll likely still be on medications, going for repeat blood tests and early scans, holding your breath at every milestone.
We’ve learned to take it one step at a time. To stay hopeful, but also realistic. And to be gentle with ourselves and allow ourselves to feel all the emotions—they are all valid.
2. Choosing the Right Fertility Clinic Can Change Everything
Not all fertility clinics are the same. Success rates, treatment protocols, costs, and patient care can vary widely. We didn’t realise just how much until we’d gone through a few cycles ourselves. At first, we didn’t know what questions to ask or what red flags to look for—but over time, we learned the hard way how important it is to be your own advocate. Here are a few things we wish we’d asked sooner.
What to ask before choosing a fertility clinic
- Talk to your clinic about success rates based on your age and medical history, not just general stats. Ask what happens if a cycle doesn’t work. You deserve transparency—and a plan for what’s next.
- Ask more questions: Why are they recommending a specific protocol? Are they tailoring treatment to your individual case? The best protocol for you depends on a combination of your unique biology and your treatment history so you should expect that different doctors or clinics may suggest new strategies or tweak protocols based on how your body responded in previous cycles. Learn more about different IVF protocols in our blog: IVF Stimulation Protocols Explained
- Look for transparency: Good clinics will explain options clearly, listen to your concerns, and involve you in decision-making.
- Don’t ignore your instincts: If something feels rushed, unclear, or impersonal, you’re allowed to walk away.
- Get thorough testing upfront—and throughout your cycle: Some clinics skip important tests early on, which can mean you’re put on a standard protocol that doesn’t truly match your needs.
- Make sure your clinic is investigating both partners and looking at potential causes of infertility from the start—including things like endometriosis, thyroid issues, sperm quality, or immune factors. Ask what testing they do as standard. Want more information on sperm quality and what to look out for? Check out our blog Sperm Quality and IVF: Understanding the Role of Male Fertility in IVF Success
- It’s also important that they monitor things during your cycle—like hormone levels or lining development—so they can make timely tweaks if needed. For example, checking progesterone levels after transfer can help spot gaps in luteal support that could affect implantation. If something feels missed, speak up. A personalised approach can make all the difference.

3. The Emotional Toll Is Real (And Often Overlooked)
IVF isn’t just physically intense—it’s emotionally exhausting. It can take over your life and relationships.
You might find yourself timing everything — holidays, birthdays, special events, even work commitments — around cycles, scans, or transfers. Suddenly, every plan turns into a “maybe”: Should we go to that wedding? Can I book that holiday? Is now the right time to apply for that new job? We’ve been there too — we missed birthdays we really wanted to celebrate, holidays we’d been looking forward to, cancelled visits from friends, and countless moments because everything revolved around treatment.
It’s also a mental minefield. You start questioning every single thing you do:
- Was that coffee a mistake?
- Should I have eaten more greens today?
- Did I take my medication on time?
- Should I be exercising more… or less?
You start doubting your body and your decisions, constantly wondering if something you did could be the reason a cycle didn’t work. It’s a heavy burden to carry, and it’s emotionally exhausting.
On top of that, the stress and anxiety can be overwhelming. The pressure to stay calm (because “stress isn’t good for fertility”) can actually make you feel worse. Please know this: you’re not doing anything wrong. Feeling anxious, scared, or constantly on edge is a completely valid response to what you’re going through.
We found it helpful to try small things that supported our mental health and ease the stress —whether it was a 10-minute walk outside, guided meditation, journaling, or simply allowing ourselves to cry when we needed to. Everyone copes differently, but finding even one way to manage IVF stress can make the process feel a little less heavy.
IVF forces you into a state of logistical and emotional limbo. Protecting your energy isn’t selfish—it’s essential. Say no when you need to. Life will wait for you. So will the people who care about you.
And don’t forget, it’s hard on your partner too. Even though they’re not the ones injecting themselves with hormones, they’re still riding the same rollercoaster. Be kind to each other and talk openly. You’re in this together.
You can read in more detail how we managed our stress and anxiety while navigating IVF in our blog Stress og angst under IVF - og hvad du kan gøre ved det
4. The Two-Week Wait Can Feel Endless
After embryo transfer, you enter the dreaded two-week wait (TWW) before taking a pregnancy test. It’s one of the most emotionally intense parts of the IVF process, and and often the hardest stretch to get through mentally.
You might find yourself obsessing over every twinge, symptom, or lack of symptom. Try not to Google every feeling—we’ve been down that rabbit hole and know how hard it is not to symptom spot. Progesterone can mimic pregnancy signs, which just adds to the confusion.
Instead, try and focus on distraction:
- Watch comfort shows
- Go for walks
- Journal or meditate
- Avoid testing early if you can unless your clinic advises it (we know all too well how hard this can be!)
This stage is incredibly emotional—full of hope, dread, excitement, and fear, often all tangled together. Whatever you’re feeling, please know it’s completely normal, and you’re not alone. We’ve been there too.

5. The Cost Adds Up Quickly
IVF is expensive—often more than people expect. Beyond the base treatment cost, you might need:
- Extra medications
- Additional blood tests or scans
- Embryo freezing and storage
- Repeat egg retrievals
Ask for a detailed breakdown of what’s included in the clinic’s price list—and what’s not. And don’t forget to budget for things like medication, supplements, travel, time off work, and emotional or holistic support (like therapy or acupuncture).
We both ended up going abroad for treatment after multiple cycles near home, which added a whole new layer of cost and logistics—flights, hotels, taxis, meals, and unexpected extras. Of course, not everyone will choose to travel for IVF, but if it’s something you’re considering, it’s important to factor those expenses in too.
Some choose to plan for multiple egg collections upfront—especially if they want to plan for more than one child or are concerned about egg quality declining over time.
6. Not Every IVF Cycle Results in Embryos or a Transfer
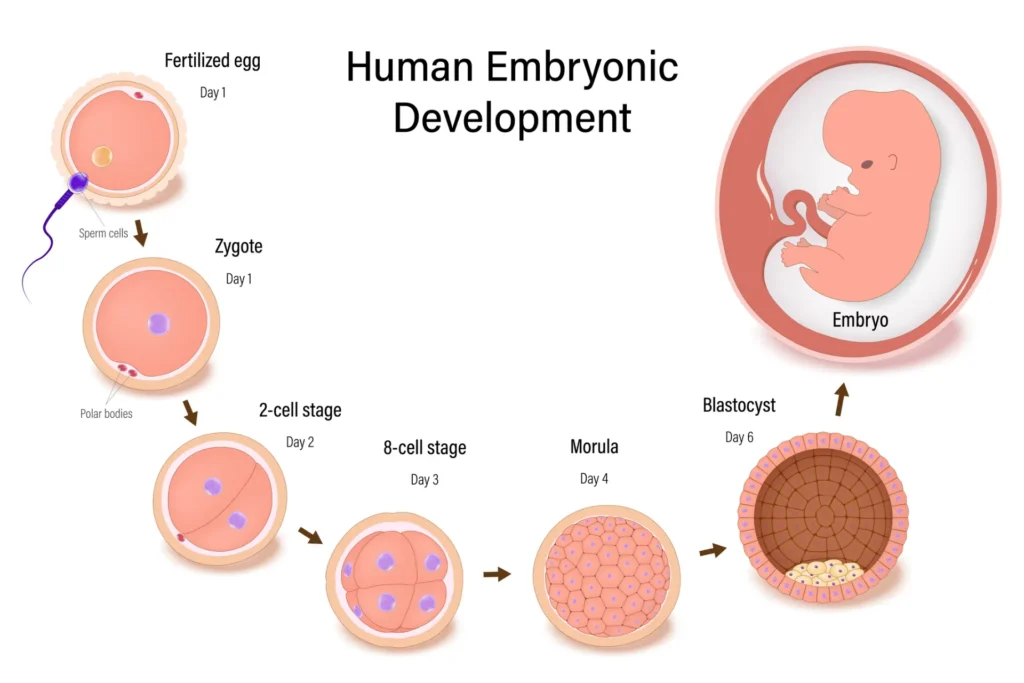
Even if your body responds well to meds and produces a good number of eggs, not all will fertilize, develop, or be genetically viable—and that’s totally normal. This took us a while to get our heads around.
Here are some typical averages:
- 70–80% of mature eggs fertilize
- 50–60% of those make it to day 3
- 40–50% of day 3 embryos become day 5 blastocysts
So if you start with 10 mature eggs, you may end up with 2–3 blastocysts—and that’s actually a good result.
For us, there were cycles at some clinics in the early stages of our journey where we didn’t even make it to the blastocyst stage. We had to transfer embryos on day 2 or day 3 because it was feared they wouldn’t make it to day 5. After months of prepping for egg collection, this felt incredibly disheartening. It’s a part of the process we weren’t prepared for—and one that made us realise just how delicate early embryo development can be.
These numbers can feel especially daunting if you’re over or nearing 40 and using your own eggs, since egg quality tends to decline with age. If that’s you, we’ve written more about what to expect and how to give yourself the best possible chance in IVF After 40 With Your Own Eggs: Personalised Treatment Through AI and Research
It can still feel like a shock when the numbers drop at each stage, especially if you were hopeful about having lots of embryos to choose from or freeze. But understanding this from the beginning can really help manage expectations and reduce heartbreak.
7. IVF Medications Can Hit Hard
The hormone meds are no joke. Between the bloating, mood swings, headaches, and fatigue, we were caught off guard by how intense it could feel—not just physically, but emotionally too.
In rare cases, some people develop OHSS (ovarian hyperstimulation syndrome), which can require extra monitoring or even treatment. It’s important to listen to your body and reach out if something doesn’t feel right.
Here’s what helped us get through the rougher days:
- Staying really well hydrated (water with electrolytes became a must!)
- Eating protein-rich foods—think lots of egg whites, chicken, fish, and bone broth
- Letting ourselves rest without guilt, even if it meant canceling plans
- Calling the clinic whenever something felt “off” instead of trying to tough it out
You know your body better than anyone else. Don’t be afraid to speak up, ask questions, or push for answers. Advocating for yourself isn’t a hassle—it’s an important part of the process.
8. Lifestyle Changes Matter (More Than We Expected)
We didn’t realise just how much everyday habits—like what we eat, how we manage stress, and even what products we use—could impact egg and sperm quality. No one really talked to us about that at the start, and we wish they had. It turns out these things can make a real difference, especially in the months leading up to a cycle.
Ideally, try to start making small, manageable changes at least 3 months before IVF, since that’s how long eggs and sperm take to mature.
Lifestyle changes that can support IVF outcomes
- Reduce alcohol and caffeine
- Eat a fertility-friendly, anti-inflammatory diet — you can read more about following a fertility-friendly diet to support IVF in our blog post: Den bedste IVF-kost: Hvordan en middelhavstilgang kan hjælpe med at forberede din krop på IVF
- Cut back on plastics, fragrance, and environmental toxins
- Prioritise sleep, gentle movement, and mental health
- Consider adding complementary therapies like acupuncture or Low Light Laser Therapy (LLLT). Read more about this in our blog posts Red Light Therapy (LLLT): The Fertility Tool You’ve Probably Never Heard Of and Can Acupuncture Improve IVF Success?
And if you’re dealing with conditions like endometriosis, PCOS, or adenomyosis, don’t wait until IVF starts to begin supporting your body. These conditions can affect your response to treatment, so taking steps to reduce inflammation, manage symptoms, and optimise your overall health beforehand can make a real difference. Even small adjustments to your lifestyle can help give your body the best possible chance.
9. Waiting Is a Big Part of the Process
IVF is full of waiting—and not just during the two-week wait. You’ll wait for your period, your scans, your bloodwork, your fertilisation report, your blastocyst update, your transfer date… and of course, for your results.
You’ll also spend a lot of time at the clinic, often with short notice. Monitoring appointments usually happen early in the morning and can be hard to juggle with work or other responsibilities. Ask your clinic what kind of schedule to expect, and see if you can get extra flexibility at work during your cycle.
And don’t be surprised if your embryo transfer doesn’t happen right away. Some people need a break between egg collection and transfer – especially if hormone levels are high or there’s a risk of OHSS. In these cases, clinics may recommend a frozen embryo transfer (FET) instead of a fresh one to give your body the best possible chance.
It might not be what you pictured, but that pause is often a sign your doctor is doing what’s best for your outcome.
10. Finding Support Makes a Big Difference
IVF can feel lonely. Even your closest friends might not understand unless they’ve been through it.
That’s why finding a support network, whether it’s your partner, someone you know who has been through it, a therapist, or an online space like The IVF Buddy where people share real IVF experiences, can be a lifeline. You need people who “get it,” and who won’t tell you to “just relax.”
If you feel safe doing so, sharing with your boss or close colleagues can also relieve pressure when you need time off or flexibility. We were lucky to have very supportive co-workers which lifted a lot of the last minute stress when planning for appointments.

Final Thoughts
We hope you found some of this helpful, whether you’re just starting IVF or already knee-deep in the process.
We wrote this blog because we genuinely wish someone had told us these things when we began. Knowing what to expect won’t take away the hard parts, but it can make you feel a little more prepared, a little less alone, and a lot more supported.
IVF is a rollercoaster—but being informed, supported, and emotionally prepared can make all the difference.
That’s why we created My IVF Buddy—to offer honest insights, practical tools, and a sense of community for anyone navigating IVF.
We’re here with you, every step of the way.
Want to Feel More Supported on Your IVF Journey?
Join our email list for insider tips, new blog updates, exclusive resources, and gentle encouragement—delivered straight to your inbox.
Looking for more honest, experience-based IVF insights and research? You might also like:
- IVF Stimulation Protocols Explained
- The Best IVF Diet: How A Mediterranean Style Approach Can Help Prepare Your Body For IVF
- Stress and Anxiety During IVF and What You Can Do About It
- Sperm Quality and IVF: Understanding the Role of Male Fertility in IVF Success
- Acupuncture and IVF: Can Acupuncture Improve Success?
- Understanding Failed FETs and How to Move Forward
- IVF After 40 with Your Own Eggs: Personalised Treatment Through AI and Research
- Red Light Therapy (LLLT): The Fertility Tool You’ve Probabky Never Heard Of



